is made up of bones (vertebrae that support the body's weight), their joints (facets that guide the direction of the movement of the spine), and the discs (which separate the vertebrae and absorb the shock as you move), the muscles and the ligaments that hold it all together. One or more of these structures can be injured:
- You can strain or sprain the ligaments or muscles from a sudden movement, improper movement, or through over use.
- You can sprain the ligamentus part of your discs.
Sprains can allows the disc to bulge & press against a nerve.
SIGNS & SYMPTOMS
Pain or deep ache of the neck, shoulder or arm(this needs to be differantiated from true shoulder pain, such as tendonitis\bursitis). There may be burning or tingling of the arm or hand or headaches. It may be continuous, or only occur when you are in a certain position. The pain may be aggravated by turning your head, looking up or looking down ( as with reading).
- limited range of motion (less than normal movement) of the neck.
- Stiffness of the neck and shoulder muscles.
Causes
- postural strain ( improper position when sitting - reading - working at a computer)
- Severe blow or fall.
- Car accident
- Heavy lifting.
- Sleeping without good neck support/sleeping on your stomach
- Turning over while you are asleep. Then waking up with a "stiff neck."
- Degenerated/ ruptured cervical disc.
- Bone spur.
- Nerve dysfunction.
- Osteoporosis, tumors.
- Spondylosis (hardening and stiffening of the spinal column).
- Congenital problem.
- Often there is no obvious cause.
Risk Increases With
- Sitting for long periods and bending your head /neck forward. (desk work, cooking, etc.)
- Participation in sports without warming up ( stretches).
- Sharp increase in athletic activity (weekend athlete)
- Poor posture with sitting - sleeping.
- Frequent travel on planes.
- Falling asleep sitting up.(head hanging down)
How to Prevent
- Exercises to strengthen /stretch neck and shoulder muscles.
- Learn how to sit and work without bending your neck.
- Proper back & neck support for your car/bed/sofa/chair.
WHAT TO EXPECT WITH IF YOU SEE AN MD:
Diagnostic Measures
- Observe your symptoms.(What makes the pain worse/better)
- Medical history and exam by a doctor & referral to a physical therapist for persistent symptoms.
- Laboratory blood studies to determine if there is an underlying disorder, x-rays of the spine, sometimes a CT or MRI scan.
- Testing (see above) is often not done unless the person is not responding to conservative (rest, medications, physical therapy) treatment.
Appropriate Health Care
- Treatment will depend on severity of the pain and discomfort.
- Acute -sudden onset of pain or severe pain - severe neck and/or arm pain may require use of a collar and/or bed rest for first 24 hours and use of ice for first 72 hours. This usually follows trauma, a car accident, a fall or sharp pain/popping felt in the neck. SELF CARE Additional treatment will be determined by severity of the problem. Recent medical studies indicate that staying more active is better for spinal disorders than prolonged bed rest.
- Chronic- slow onset(over months or years) or low grade pain(constant dull ache). This may respond best to heat. If you are not getting relief with heat, try ice.
- Physical therapy treatment should address risk factors, prevention & a home exercise program in addition to pain reduction treatments.
- Physical therapy should be prescribed when you have been treated by your M.D. but pain persists beyond 1-2 weeks or if you have had multiple episodes of pain over the past year.
- In most states you can go directly to a physical therapist. Depending on the nature of the condition, the therapist may refer you to a physician . The physician can prescribe medications, order tests and check to be sure you do not have a more serious medical condition that may be causing your symptoms.
- Physical therapy treatments should address risk factors, prevention & a home exercise program in addition to pain reduction treatments. SELF CARE.
- A physical therapy evaluation should include:
- History( The therapists will ask: How did you hurt yourself, When did the pain first appear? What makes the pain worse/better? Have you had this type of pain before? What were you doing just before you felt pain? What does your daily routine involve? etc.)
- Physical exam: ( You will be asked to do certain movements to determine what movements increase your pain, Your posture - how you sit & stand - will be evaluated, Your muscles will be palpated(massaged) to look for painful "knots" or spasm (increased tension), The mobility and quality of the motion of your joints will be checked, Your may have your reflexes tested, etc.
- Physical therapy treatments will vary depending on the condition. A through treatment will include a few basic elements:
- Pain reduction may include use of heat, ice, massage, relaxation, stretches, joint mobilization and other modalities including ultrasound & electric stimulation.
- *A home program may start out as simple as a list of things to avoid. This should increase gradually as you progress to include exercises, stretches and some type of simple first aid. The goal is for you to gain control over the symptoms as you gradually eliminate the cause of the problem. * This is where physical therapy differs from traditional chiropractic care.
- Prevention includes:
- discussing risk factors for your specific condition.
- exercises to increase strength and flexibility.
- training in how to sit, stand, bend, move, return to sports, etc. without re-injuring yourself.
- Suggestions for basic equipment including chairs, lumbar supports, wrist rests, etc. Depending on the person and the condition this may require purchasing a few items. Many "lumbar supports" can be made from simple items in the home such as pillows, towels, blankets. ( Your jacket can work as a lumbar support if you are out and you run into an unfriendly chair.)
- Options are available such as physical therapy, acupuncture, orthopedic care, treatment by a chiropractor, physiatrist or neurologist and others including surgery for damaged disk, or a local injection(epidural).
- Massage may help. Be sure the person is well trained or the massage may cause more harm than help.
- HOME TREATMENT The goals of self-care are to relieve pain, promote healing and avoid re-injury. For the first two or three days: Immediately after an injury and for the next few days, the most important home treatments include:
- Ice pack or cold massage applied to the low back for ACUTE strains Get in a comfortable position and apply cold packs or ice for 15-20 minutes three or four times a day or up to once an hour for at least the first three days. Cold decreases inflammation, swelling and pain.
- Heat applied for 15 -20 minutes while resting in a comfortable position with heating pad or hot water bottle for CHRONIC strains . Use caution with heat as this can increase swelling. If you are not getting relief with heat you may respond better to ice. SEE DEFINITION OF ACUTE VS CHRONIC.
- Use a cervical pillow. If you don't have a cervical pillow use a feather pillow with a small towel roll tucked in to support your neck. Everyone is different if you have a "good" pillow you will feel better after resting. If you have a "bad" pillow you will feel worse after resting.
- Use of a collar.
- Learn stress reduction techniques, if needed.
- Take breaks if you have to stand or sit for long periods.
- Sit or lie in positions that are most comfortable and reduce your pain, especially positions that reduce arm or hand pain.
- Do not sit up in bed, and avoid soft couches and twisting positions. Avoid positions that worsen your symptoms, such as sitting for long periods of time.
- Bed rest can help relieve neck pain but may not speed healing. Stick with what makes you feel better. Unless you have severe arm pain, one to three days of rest should relieve pain. More than three days is not recommended and could actually delay healing. Try one of the following:
POSTURES FOR ACUTE PAIN RELIEF
- Lie on your back with a soft(feather) pillow and a small towel roll under your neck with your knees bent and supported by large pillows.
- Lie on your side with a soft (feather) pillow and a small towel roll under your neck.
- When you sit add pillows so you can rest your head back comfortably and place a pillow under your arms.
- How big should the pillow be? Exactly where do I put the pillow? Use what gives you the best pain relief. ( We are all a little different.)
- Good posture means ear, shoulder & hip are in a straight line - this is the same for standing, sitting & lying down.
Which excercises are for you?
- If you have injured your neck within the last two weeks, or you have more pain in you arm/hand than in your neck, see First aid for back pain.
- Discontinue any exercises that increase pain or that causes pain to move towards the hand (i.e.: pain moves form shoulder to arm or arm to hand).
- Gradually increase any exercise that helps you feel better. STRETCHES
EXERCISES TO AVOID Many common exercises actually increase the risk of low neck pain. Avoid the following:
- neck circles.
- bending neck forward or looking up.
FIRST AID FOR NECK PAIN stop any exercise or treatment that increases your pain. When you first feel a catch or strain in you neck, try these steps to avoid or reduce expected pain. These are the most important home treatments for the first few days of neck pain.
First aid # 1 ICE As soon as possible, apply an ice pack to the injured area. (10-15 minutes every hour). Cold limits swelling, reduces pain and speeds healing.
First aid # 2 MEDICATION Some medications are available without a prescription. If the non-prescription dose does not relieve your pain CALL YOUR DOCTOR. Take aspirin or ibuprofen reglularly as directed on the bottle(call your doctor if you've been told to avoid anti inflammatory medication). Acetaminophen (tylenol) may also be used. Take these medications sensibly; never exceed the dosage suggested on the bottle, the maximum recommended dose will reduce the pain. Masking the pain completely might allow movement that could lead to re-injury.
First aid # 3 CHANGE POSITION FREQUENTLY Take the time to add a small pillow or towel roll to support your head/neck when you are sitting or lying down. DON'T STAY IN ANY POSITION THAT INCREASES YOUR PAIN.
First aid # 4 RELAX YOUR MUSCLES Listen to soft music - Practice deep breathing - try one of the commercially available relaxation tapes.
First aid # 5 USE A COLLAR USE A COLLAR A soft collar can help to rest your neck. This should be used for short periods .(Not more than an hour at a time. - take it off after the first fifteen minutes to be sure it does not increase your pain - Not more than a few days.)
First aid # 6 STRETCHES When to see M.D.
DO NOT CONTINUE WITH ANY EXERCISE THAT INCREASES YOUR PAIN. YOUR SHOULD FEEL A GENTLE STRETCH TRY TO RELAX.
- SIDE STRETCHES
- Sit or stand in a comfortable position
- Move your head slightly to one side, bringing your ear closer to your shoulder
- Keep your shoulders down
- Relax and hold for 5-10 seconds
- Stop if pain is increased or has moved into the arm or toward the hand.
- CHIN TUCK
- Sit or stand in a comfortable position
- Pinch your shoulder blades together
- Bring your chin back so it is in line with your shoulder and hip(see picture)
- Keep eyes level - do not look up or down
- This is a very small movement of your head, do not push back too hard.
- Keep your shoulders down
- Relax and hold for 5-20 seconds
- Stop if pain is increased or has moved into the arm or toward the hand.
- TURNING
- Sit or stand in a comfortable position
- Turns your head slowly to one side.
- Keep your shoulders down.
- Relax and hold for 5-10 seconds.
- Stop if pain is increased or has moved into the arm or toward the hand.
- Do the first aid exercises three to four times a day .
After two or three days of home treatment:
- Slowly increase the frequency of the first aid exercises.
- When your pain is gone slowly resume normal activities. Continue to use caution with lifting, bending, sitting & sports for 6 - 8 weeks, after the pain is gone, to allow the neck to heal. If you have a regular exercise program begin easy exercises that do not increase your pain. Start with 2-5 repetitions twice a day and increase to 10 as you are able.
- Try to continue with daily work or school schedules to the extent possible. Use care in resuming normal activities. Stop activities that cause increased pain.
- A gradual stretching/strenghtening program can help reduce pain. (Use caution - sometimes you don't feel pain until the day after you exercise.)
- Physical therapy is indicated for Acute ( severe ) pain that does not respond to bed rest or for Chronic ( less severe, but lingers over several weeks/months years) pain. Physical therapy can be prescribed by your doctor and is generally covered by insurance. A physical therapist is licensed to treat you without a doctor's prescription but in many cases he/she may advise you to see a M.D. to rule out a more serious problem. Generally, physical therapists and M.D.'s work together to provide you with the best care.
- Avoid strenuous activity for 6-8 weeks.
- After healing, continued use of good body mechanics (good posture with sitting, standing, bending, driving and resting) can prevent future problems. A physical therapist can instruct you in a basic program of back care including maintenance exercises and a first aid program to prevent a minor injury from becoming a major injury.
POSITIONS TO AVOID Many common activities actually increase the risk of neck pain. Avoid the following:
- Sleeping/resting on the couch with your head on the arm rest.
- Falling asleep in your chair or in your car without support for your head.
- Aviod looking down (working at a desk) or looking up (painting a ceiling, looking at something on a high shelf.) for prolonged periods.
Possible Complications
Chronic neck pain and restricted lifestyle.
DONT LIVE WITH PAIN - THERE ARE SIMPLE TREATMENTS INCLUDING SLOWLY PROGRESSIVE EXERCISE PROGRAMS THAT CAN HELP MOST EVERYONE WITH CHRONIC NECK PAIN. THIS IS USUALLY COVERED BY INSURANCE. IF YOU NEED HELP A PHYSICAL THERAPIST CAN ASSIST WITH REDUCING PAIN AND SETTING UP A HOME PROGRAM.
You have mild, neck pain that persists for 3 or 4 days after self-treatment .
- Neck pain or arm pain is severe.
- Neck pain or neck and arm pain that goes away for short periods but keeps coming back.
- New or unexplained symptoms appear.
- Physical therapy should be prescribed when you have been treated by your M.D. but pain persists beyond 1-2 weeks or if you have had multiple episodes of pain over the past year.
Probable Outcome
Gradual recovery, but back troubles tend to recur. A home program can prevent continued neck problems.
Physical therapy can help you prevent long term problems.
 Dizziness, nausea, "migraine" and "sinus". Because of its intimate involvement with brain stem and the vagus nerve, the SCM muscle of the neck produces a long list of neurological and pain symptoms which appear primarily in the head and face but which may also appear as nausea, motion sickness, and balance problems.
Dizziness, nausea, "migraine" and "sinus". Because of its intimate involvement with brain stem and the vagus nerve, the SCM muscle of the neck produces a long list of neurological and pain symptoms which appear primarily in the head and face but which may also appear as nausea, motion sickness, and balance problems. 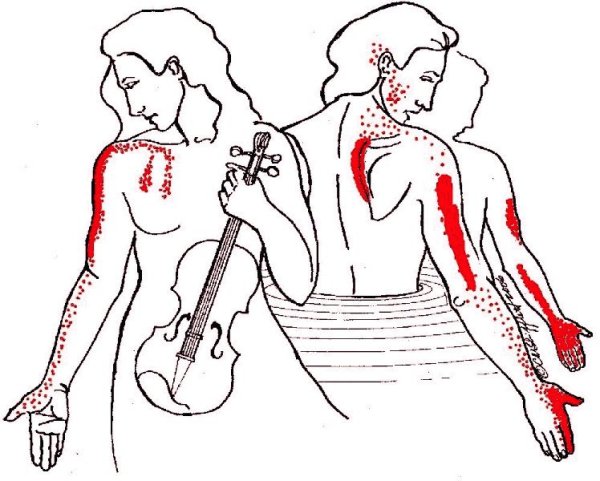
 It refers pain to both upper and lower molar teeth, causes TMJ dysfunction, earache and a "sinus" pain over the eyebrow.
It refers pain to both upper and lower molar teeth, causes TMJ dysfunction, earache and a "sinus" pain over the eyebrow.  Combine a head-forward position with a pipe and long hours of playing the violin (see the scalene pain pattern, above) and what do you get?
Combine a head-forward position with a pipe and long hours of playing the violin (see the scalene pain pattern, above) and what do you get? 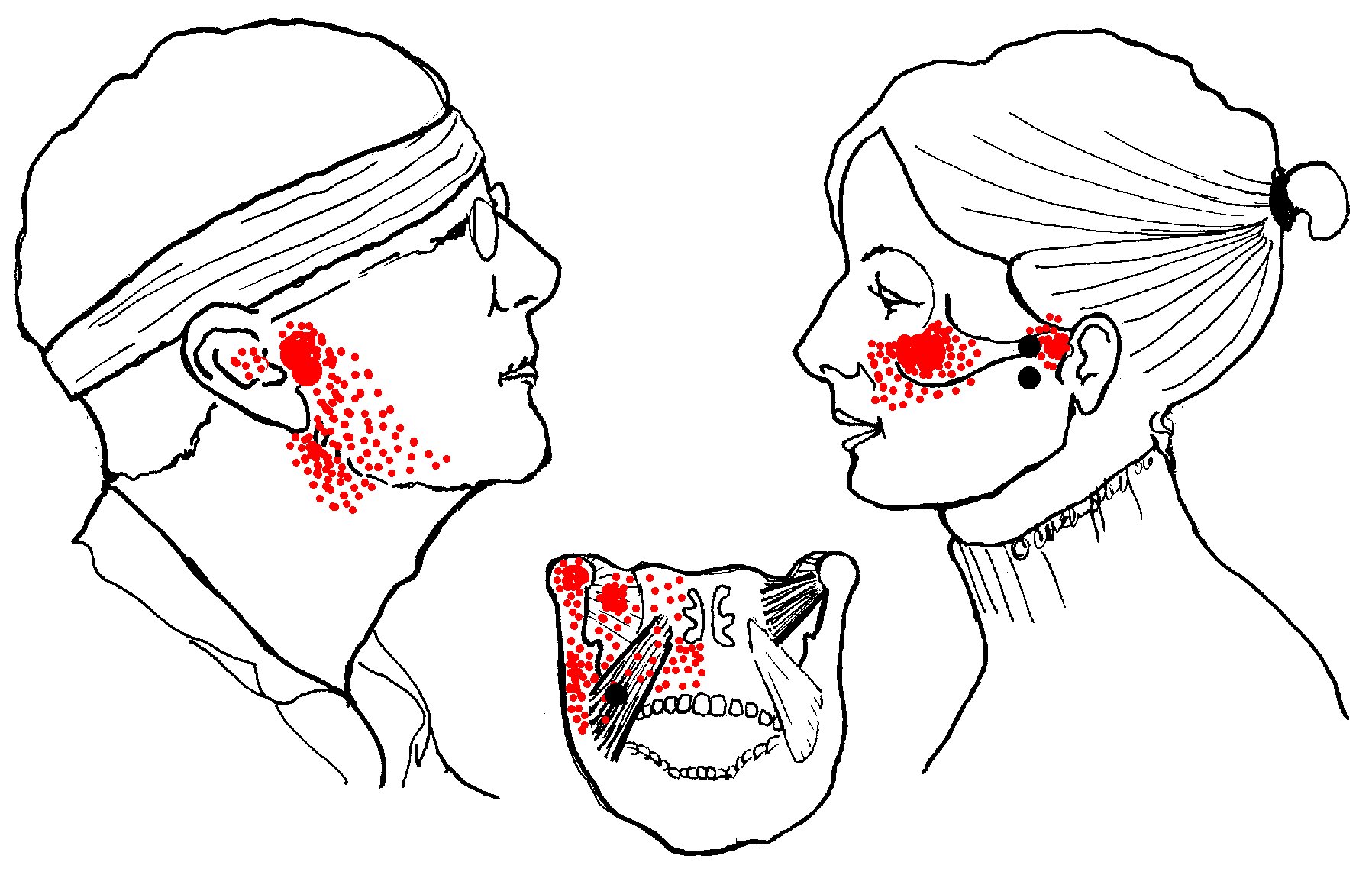
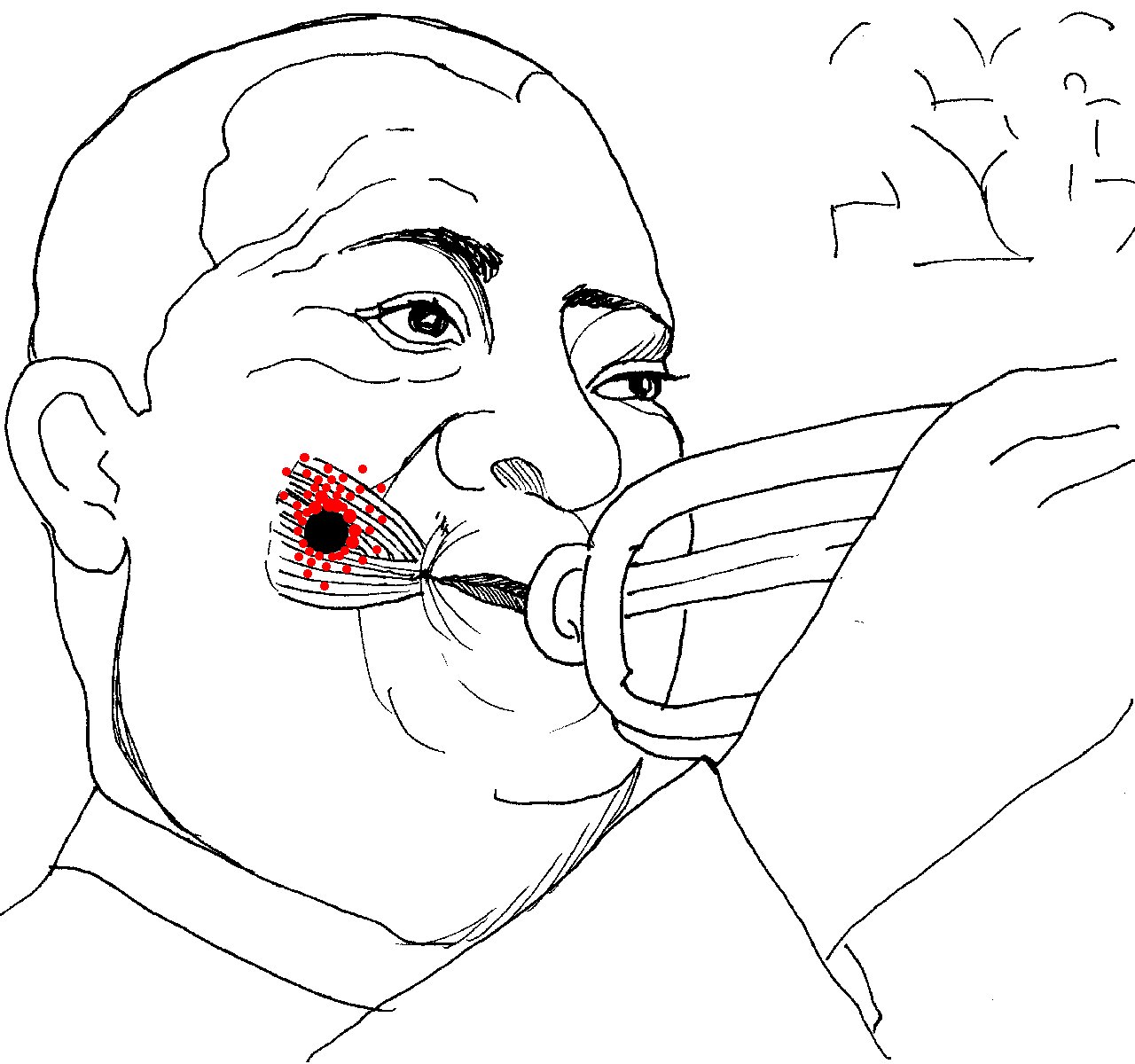 the part of the cheek that puffs out when playing the trumpet (for which it is named), blowing up balloons or stuffing one's mouth too full. Buccinator pain may appear suddenly following dental/orthotic work.
the part of the cheek that puffs out when playing the trumpet (for which it is named), blowing up balloons or stuffing one's mouth too full. Buccinator pain may appear suddenly following dental/orthotic work. 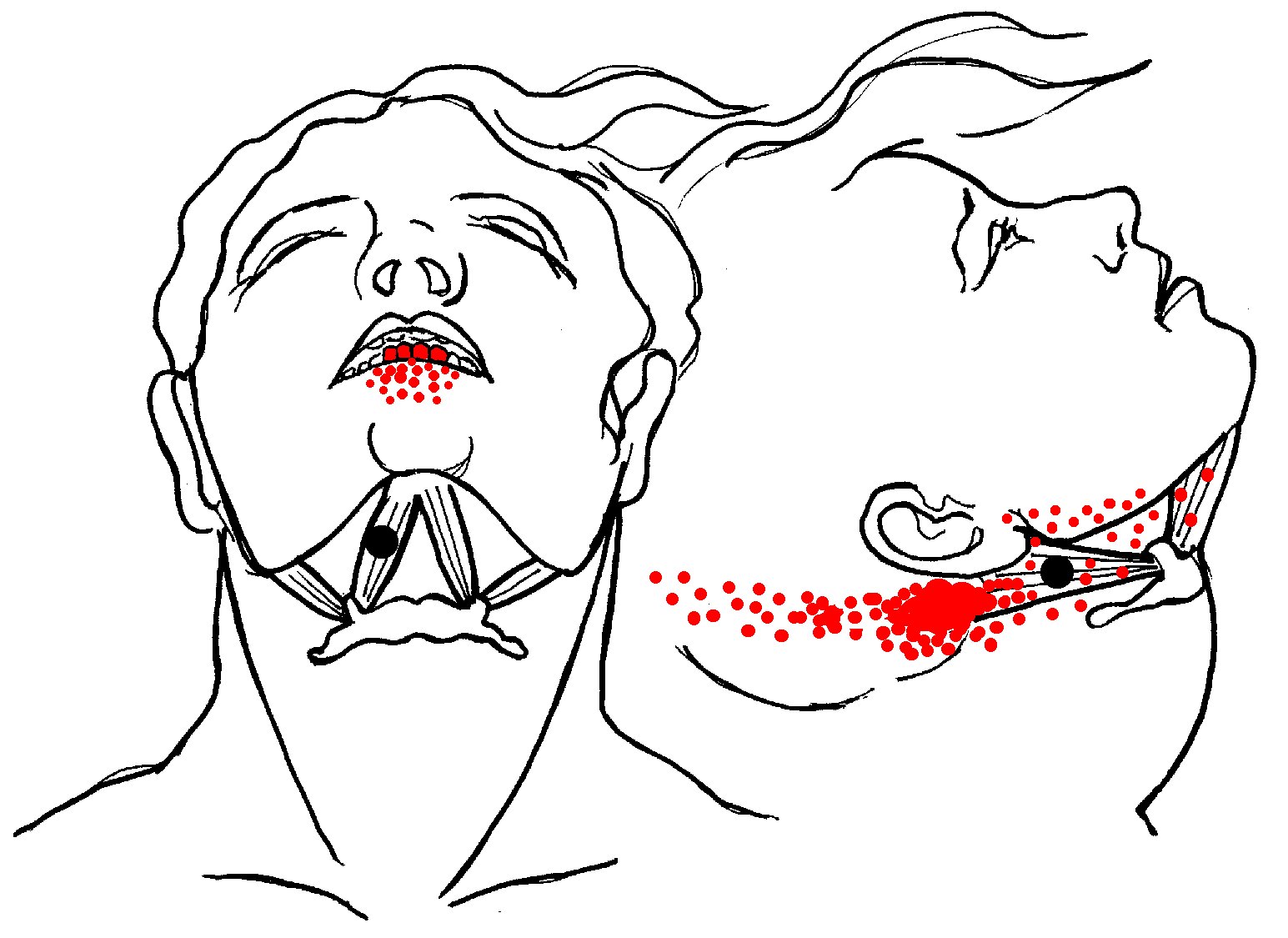 Strained by retrusion of the jaw (as in playing the clarinet or similar wind instruments) or by holding a violin in place with the chin. Commonly damaged in whiplash injuries in concert with other neck muscles such as trapezius and splenius.
Strained by retrusion of the jaw (as in playing the clarinet or similar wind instruments) or by holding a violin in place with the chin. Commonly damaged in whiplash injuries in concert with other neck muscles such as trapezius and splenius. 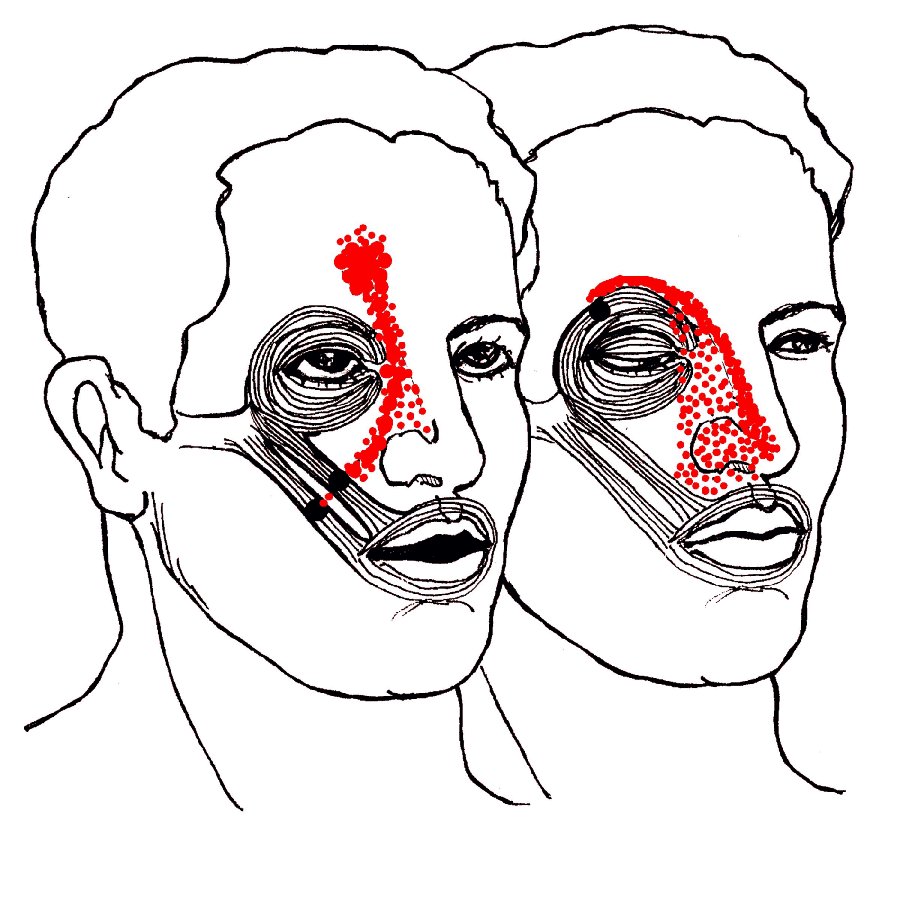
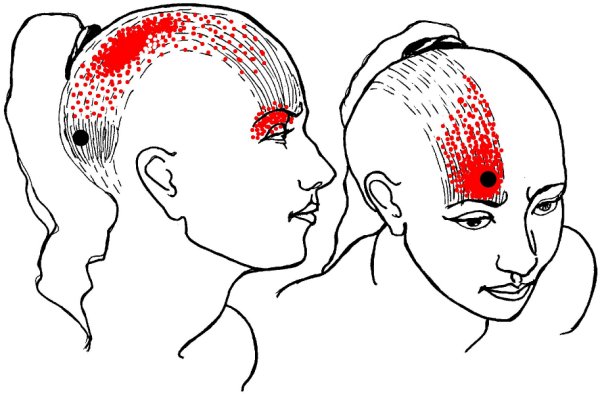
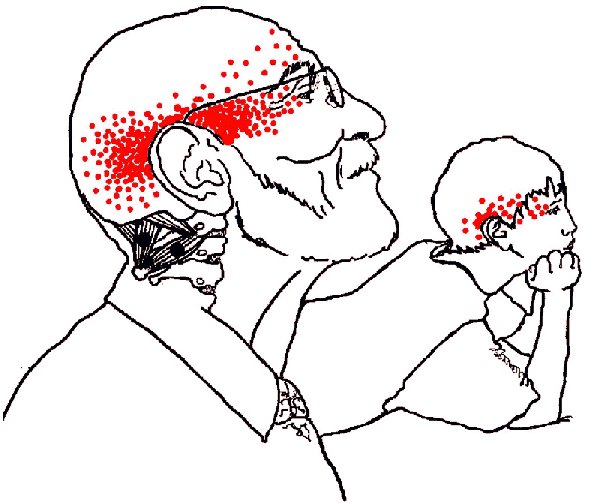 The four pairs of suboccipital muscles cause deep aching pain running in a band from the back of the head to the orbit of the eye, possibly with balance problems and dizziness.
The four pairs of suboccipital muscles cause deep aching pain running in a band from the back of the head to the orbit of the eye, possibly with balance problems and dizziness.  Pain from this muscle also appears in the sacrum at the sacro-iliac joint and then reappears in the face and jaw where it may fire off symptoms of TMJ and toothache.
Pain from this muscle also appears in the sacrum at the sacro-iliac joint and then reappears in the face and jaw where it may fire off symptoms of TMJ and toothache. 